Medicolegal Monday, March 29, 2021
Over the years, I’ve been asked to review multiple lawsuits resulting from complications during pediatric airway management. After all, hypoxia resulting from critical respiratory events is the most important reason why children develop brain damage in the hospital setting. Invariably, these cases were not managed by anesthesia professionals, but rather by other types of healthcare providers (e.g., pediatricians, nurse practitioners, adult ER docs, etc.) tasked with emergency resuscitation of (mainly) infants in different settings, such as emergency rooms, NICUs, and labor & delivery suites. The one thing they all have in common is the inability to oxygenate, either because of technical difficulties with tracheal intubation, or failure to bag-mask ventilate adequately. So, I thought this would be a good opportunity to review six important lessons I’ve learned from evaluating these cases that can be adopted by even the most expert pediatric anesthesia providers:
1. Know PALS and the Neonatal Resuscitation Algorithm. Cold. Make sure your certificates never expire. Those certificates are good for two years, but each institution should perform simulations at least yearly for all their staff. In pretty much every case I’ve reviewed, the plaintiff’s attorney will ask the defendant about their certificate status at the time of the critical event that led to the complication. Even after you have renewed your certificates, make sure you always have a handy reference immediately available, in the form of an OR wall poster, pocket-sized handbook, or others. There is no reason why any of us has to memorize certain details of critical incident treatments, especially in the midst of a stressful crisis. The Society for Pediatric Anesthesia has a great app (Pedi Crisis) that can be found here. Take advantage of this valuable resource and download it now.
2. Know any of the many published Pediatric Difficult Airway Algorithms. Cold. Most of these algorithms are similar, with a few slight differences. Here’s one published by a multidisciplinary team at the Children’s Hospital of Philadelphia, and here’s the official ASA version, applicable to both adults and children. This should also be immediately available in every OR and other anesthetizing or critical care locations.
3. If hypoxia-induced bradycardia occurs, the drug of choice is not atropine or epinephrine, it’s oxygen. If oxygen is not transferred into the patient’s lungs the bradycardia will not resolve. In every case I’ve reviewed, the defendant has sworn that the patient remained bradycardic even though they were achieving adequate bag-mask ventilation. Unless the hypoxia has been so profound and of enough duration to cause cardiac ischemia, this cannot be the case. Even seasoned professionals may have difficulty discerning adequate lung inflation with bag-mask ventilation. Although there can be a lag between getting the oxygen to the brain/heart and resumption of normal sinus rhythm, one must always assume that bradycardia means hypoxia.
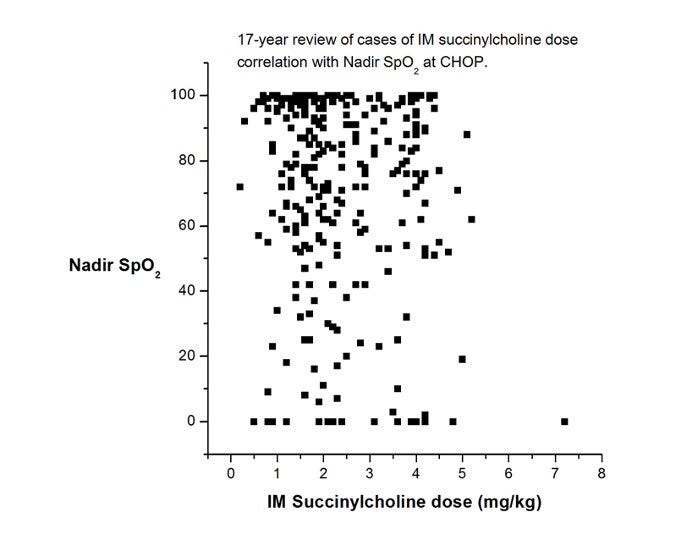
4. Use succinylcholine sooner rather than later. While I realize this statement will have its detractors, I’m convinced that succinylcholine has saved more lives and brain cells than any other intervention we have for life-threatening hypoxemia. Sure, it has side effects, but they are nearly always manageable and secondary to brain damage. If the patient already has an indwelling IV, very small amounts of succinylcholine (0.1 mg/kg) have been reported to be effective. If an IV has not been placed, IM succinylcholine is also effective. How much to give? The most often cited reference (Liu et al, 1981) recommends 4 mg/kg. A few years ago, one of our great fellows, Mike King, looked at our dose experience of IM succinylcholine at CHOP over 17 years. He generated this (unpublished) chart, which shows that most administrations were not as high as 4 mg/kg. But, the more you give, the faster it will work (BTW, those really low sats certainly look scary, but not one child in this time period was harmed, and I’ll bet anything that your children’s hospital has a very similar graph.)
5. Place your favorite supraglottic airway (SGA) sooner than later. Don’t wait because you think you can mask ventilate, and don’t perseverate trying to intubate. In our anesthesia world, this has become second nature to us. But surprisingly, it’s not yet become routine in other areas such as the NICU or delivery room. SGA placement is now included in the most current version of the PALS guidelines, but it is still absent in the most current neonatal resuscitation guidelines.
6. As we discussed in a previous Medicolegal Monday, think about tracheostomy sooner than later. In Complications, A Surgeon’s Notes on an Imperfect Science, Atul Gawande describes a horrific scene of a trauma victim in the ED who rapidly developed hypoxemia and required multiple attempts to secure the airway. Although he thought of tracheostomy at that moment, as the trauma resident responding to the scene, he was too shy to insist on it, and that indecisiveness contributed to a poor outcome.
And on that note, as always on Mondays,
“Let’s be careful out there!”
